Advice
Sexual Health
Looking after your sexual health is an important part of your mental and physical health, as well as your social and emotional well-being. City and Hackney have a range of sexual health services and support organisations available in the borough.
Sexual Health Services in City and Hackney
We have clinics and services throughout the City and Hackney.
You might want to visit a Sexual Health Service if:
- You have or you have not had sex yet
- You have any questions about sex, relationships or your body
All of our services are free and confidential. You can access sexual health services in a number of ways. Click the following headings to find out more:
 1. Visit your nearest young person’s walk-in clinic (no appointment needed)
1. Visit your nearest young person’s walk-in clinic (no appointment needed)
When you visit a sexual health service you can talk to the team about anything. This might be things like:
- You want free condoms
- You would like contraception to prevent pregnancy
- You have had sex and you want emergency contraception
- You have noticed something on your penis or vagina and you would like us to check whether it’s normal
- You have noticed symptoms which suggest a sexually transmitted infection
- You would just like a check-up
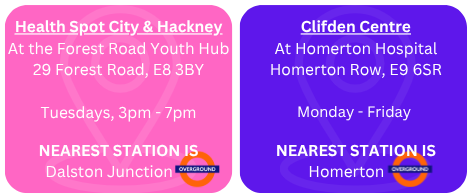
Sexual Health Clinics in City and Hackney with a dedicated young people’s service are:
At these two sites you can get: STI Tests, Emergency Contraception, Advice, Condoms, the Pill, Implant and Treatment.
If you’ve never been to a sexual health clinic before, here is a video that shows you what it’s like.
 2. Book an appointment
2. Book an appointment
Some people prefer to book an appointment rather than walk-in. If you prefer to book an appointment click on the links below:
You can also call Homerton Sexual Health Service on 0207 683 4103 to book an appointment.
 3. Free condoms and lube
3. Free condoms and lube
If you’re under 25 and live, work or study in Hackney or the City of London, you can get free condoms and lubricant through our Condom Distribution Scheme.
Register here for the scheme and pick up condoms from your local pharmacy.
Visit our webpage to find out more including a list of participating pharmacies.
 4. Order an online STI test here
4. Order an online STI test here
Sexual Health London (SHL) offers FREE STI tests to anyone living in London. This is completely confidential and you can even have the test sent to a nearby pharmacy if you prefer.
More information about what to expect is found on the SHL website – click here to register, request a kit or find out more.
More information about:
 Contraception
Contraception
A range of contraception is free and available on the NHS. There are lots of different types of contraceptives to choose from, depending on you and your lifestyle. The NHS website has information to help you choose what might be best for you.
Some commonly used contraceptives include:
 |
 |
 |
 |
 |
 |
 |
 |
 STIs
STIs
Sexually transmitted infections (STIs) are infections passed from one person to another person through any sexual contact. Anyone can get and pass on STIs, you don’t need to have lots of sexual partners. Some STIs don’t show any symptoms therefore it’s important to get an STI test when you’ve had sex without a condom, a change of partner, or if you’ve been told (or are worried) someone you have had sex with has an STI. The only way to know if you have an STI is to get a test or see a healthcare provider.
Getting tested means you – and your sexual partners – can access treatment quickly, if you need to. The quicker you access treatment, the less severe any symptoms are likely to be. To help lower your risk of getting an STI if you do have sex:
-
Use a condom every time you have sex (vaginal, oral, or anal).
-
Get tested with any new partners before having sex.
Common types of sexually transmitted infection (STI)
There are different types of sexually transmitted infection (STI). Click on the buttons below to find out more about:









 Confidentiality
Confidentiality
Sexual Health services are totally confidential. You don’t need your parents’ permission and you don’t have to tell them if you don’t want to. You will not have any information about your attendance at these services passed on to anyone outside of the sexual health services (like your parents, teachers, social workers, etc.) without your knowing about it and agreeing to it. In exceptional circumstances, where you or someone else is in a dangerous situation and telling someone else about this may prevent you or them from being harmed, a member of staff will be required to pass on information without your permission. However they would still inform you of what they were going to do.
 Feeling ready for sex
Feeling ready for sex
Taking the step to have sex can be a big decision to make. Everyone will make the decision at different times and what is important is making the decision at the right time for you. You are the only person that can make the choice to have sex and you should never feel pressured into having sex when you choose not to. Things to consider If you are considering having sex for the first time or having sex with a new partner, here are some things to think about:
 It’s your decision
It’s your decision
Remember only you can decide whether or not you want to have sex and it’s ok to say no.
People start having sex at different times. Just because other people are, doesn’t mean you have to.
 No means no
No means no
You shouldn’t pressurise or be pressured by someone to have sex.
You must respect someone’s decision and they should respect yours.
Yes once doesn’t mean yes always.
 Talking and getting advice
Talking and getting advice
To help you get the information you need before or after having sex, you might want to talk to a trusted adult about your thoughts and feelings.
This could be a parent/carer, a youth worker, your GP, a sexual health nurse, a teacher or anyone else that you trust.
It is also important to talk to your partner about sex, and make sure you are on the same page. It’s helpful to talk about things like safe sex and consent within this conversation.
 Being comfortable
Being comfortable
You might not be ready to have sex if you feel embarrassed or uncomfortable talking about any of this with your partner.
Talking will help you understand each other’s likes and dislikes and boundaries. What one person likes might make another person uncomfortable.
Safe sex
 Choosing my doctor
Choosing my doctor
When you go for an appointment or walk-in, ask at reception if you would prefer to be seen by a doctor/nurse of the same sex as yourself. They will try to accommodate your request depending on clinic staffing that day. If you call in advance to book an appointment, often they can try to arrange for you to see a doctor of the same sex.
 Cost of treatment (it’s free!)
Cost of treatment (it’s free!)
Your visits to the sexual healthcare clinic are always free, including any medication you might receive, or any long-term contraception methods you might choose to have ( like an implant or IUD). If you are under the age of 25, you can also pick up free condoms from your local pharmacy. Visit our website to register and find your closest participating pharmacy.
 STI Tests
STI Tests
All the tests we do are usually painless but may cause some discomfort depending on your symptoms. The tests we may recommend include urine tests (this means wee), swabs or blood tests. A swab is like a long cotton bud that is used to take a sample from the infected area (this could be from your mouth, anus or genitals). Some people don’t like blood tests in general and find this stressful. Our colleagues will be very sympathetic so don’t feel embarrassed and make sure you let them know. They will do everything they can to put you at ease.
 Feeling embarrassed
Feeling embarrassed
Some people feel embarrassed talking about sex, that’s normal. But you don’t need to be embarrassed especially when talking to a member of a sexual health team. All of our staff deal with sexual health issues every day and specialise in this area – in short, they’ve heard it all before! Our staff will always be non-judgemental and respect your privacy and dignity.
 Pregnancy (or potential pregnancy)
Pregnancy (or potential pregnancy)
If you have missed a period, or if your period is late, you can take a pregnancy test to find out if you are pregnant. You can buy home pregnancy tests in most pharmacies and supermarkets. These are usually done by peeing on them and you must follow the instructions carefully and correctly. You can also visit a sexual health clinic or your GP to have a free test and discuss your options. Depending on your situation, the medical professional may ask you for a urine test, blood test or both to get the most accurate result. Missing a period or being late doesn’t always mean you’re pregnant. Stress or changes in your lifestyle can affect your period and monthly cycle too. Get tested to be sure, and continue to use contraception if you’re still having sex and don’t want to become pregnant. If you take a pregnancy test, the result will be confidential – no matter if it is positive or negative. If the pregnancy test is positive, the experienced nurses will be able to consult you on your choices – be it termination or continuing the pregnancy. This information will not be passed on to your GP or your parents, and our healthcare professionals are able to join you if you decide to share the news with your family.
 Consent and the law
Consent and the law
Any sexual contact without consent is illegal regardless of the age of the people involved. In the UK, the age of consent for sexual activity is 16. However, just because you’re 16 or over, it doesn’t mean you have to start having sex – it’s different for everyone
 LGBTQIA+ services and support
LGBTQIA+ services and support
All of our Sexual Health Services in City and Hackney are here to support the LGBTQIA+ community. If you’d like more information about gender or sexuality, or other support for LGBTQIA+ people, you can also visit the Brook pages on gender or sexuality or the LGBT Switchboard for more information.
In Hackney, we also have a fantastic local LGBT Youth Service for young people aged 16-25, called Project Indigo.
 Emotional wellbeing and mental health support
Emotional wellbeing and mental health support
There is lots of different types of support for emotional wellbeing and mental health available across City and Hackney. You can visit the CAMHS Alliance website for more information about the different services available across the borough.
You can also get free, safe and anonymous support from Kooth.com or by calling Childine at 0800 1111.
Remember, we all have mental health and it’s important to look after your wellbeing. You can get ideas on how others are looking after their wellbeing by visit the ‘Five to Thrive’ website.
 Mythbusting
Mythbusting
You may have heard or seen information which is misleading and incorrect and could therefore affect your sexual health and wellbeing. It’s important to know the facts from the myths to help you and your partner stay safe. Check out some common myths and misconceptions below:
- Withdrawal before ejaculation – Pre-cum (fluid that comes out of the penis before ejaculation, often to help lubricate the penis) can contain sperm, therefore this is not a reliable method if you don’t want to get pregnant. Pre-cum can also contain STIs! Even shallow insertion of the penis into the vagina (sometimes called dipping) carries risks for both partners.
- You can’t get pregnant the first time you have sex – This is not true. You can get pregnant even if it’s your first sexual intercourse.
- Using cling film – Many people think that wrapping cling film, or other types of plastic barriers (such as crisp packets) around the penis will work the same as using a condom. This is not true.
- Having sex while on a period – Sperm can remain in the body for five days after sex. Even if you are on your period, your ovulation cycle can still be irregular, which means you could be at increased risk of pregnancy (ovulation is when your body releases egg cells). This is therefore not a reliable method.
- Using two condoms – Many people think using two is better than one, but not when it comes to condoms. Two condoms will rub against each other and this can weaken or break the condom. This is the same regardless of the type of condom. Use one at a time.
Other sources of information
- The NHS Sexual Health Hub has lots more answers to questions you might have on their website.
- Brook, a national charity for young people’s sexual health, also has lots of great information on their website.
- Or come in and speak to one of our friendly sexual health nurses at a clinic near you who will be happy to answer any questions you might have.